- For many teenagers who have complaints of excessive daytime sleepiness, the chief complaint is often voiced by people other than the patient (parents, coaches, teachers).
- Patients may experiencing excessive daytime sleepiness and vague feelings of weakness that would suggest a central hypersomnolence disorder. Sometimes they report “clumsiness” or “vibrations” with laughter.
Mason's Story
Our next patient is Mason. He’s a 15-year old African American teenager who has been followed in the practice since infancy. He lives with his mom, dad, and an older brother who moved away a few months ago to begin college. At his visit to the primary care provider today, Mason’s mother tells the provider that Mason STILL has trouble with sleeping a lot. At his sleep-away football camp for the varsity team, Mason’s coach had to call his parents and ask permission to have him drug-tested, because he fell asleep almost every time they were watching films of other teams. Mason even fell asleep in church last month and the pastor noticed!
Looking over the chart, it seems this has been a chronic complaint for the last 4 years. Prior notes reflect that Mason and his mom have received handouts on sleep hygiene and this has been discussed repeatedly. Today, one of Mason’s concerns is that his football coach says he needs to stop “freezing up” when the ball is snapped, or he’ll be stuck on the junior varsity team instead of varsity. Mason enjoys football and since he’s on the heavier end of the growth chart, the exercise is good for him. He really wants to be on the varsity team!
One of Mason’s mother’s biggest complaints today is that he seems to be struggling in his math class, which is a bit unusual. He did well in 9th grade geometry, but he seems to be struggling in 10th grade Algebra 2/Trigonometry class. Mason’s mother recently met with the teacher about this, and the teacher reports Mason seems engaged and interested but fell asleep during the first 3 quizzes of the school year, resulting in a low grade. When asked about this, all Mason can say is “I don’t know, I just fall asleep sometimes.”
Mason’s mom asks the primary care provider if Mason should quit football since maybe he is “doing too much and getting too tired.”
BEARS Screening for Hypersomnolence
As part of the clinic’s routine protocols all patients are screened with a BEARS assessment tool. Open the categories below to review some of the history that was obtained from Mason and his mother.
Mason reports that he falls asleep within 10 minutes. When he is really tired, he thinks he sees his football coach standing over his bed as he falls asleep.
Expert Insights
- Mason’s rapid ability to fall asleep may be a sign that points to his underlying disease
- His vision of his coach standing over his bedside is likely a hypnagogic hallucination.
Mason reports that he falls asleep a couple of times per day at school. He usually falls asleep in third period and again after lunch. He says he feels well refreshed after even a short nap in school.
Expert Insights
- Falling asleep during the day is the hallmark of hypersomnolence disorders.
- In contrast to insufficient sleep syndrome, or sleep disordered-breathing, patients with narcolepsy usually awake feeling refreshed after as short as a fifteen to thirty minute nap. Patients with other causes of daytime sleepiness do not improve as rapidly from a short nap.
Mason notes that he is a very light sleeper and wakes up frequently throughout the night. He does not have any trouble falling back asleep.
Expert Insights
- Patients with hypersomnolence due to sleep-disordered breathing will frequently report waking up multiple times per night. They will sometime note trouble falling back asleep.
- Patients with narcolepsy will often have very fragmented, light sleep. They typically have little trouble falling back to sleep and may report having very vivid dreams.
Mason reports going to bed as soon as he can after football practice, dinner, and homework.
During the school week, Mason typically goes to bed between 9:30 and 10:00PM. He gets up at 6:30 AM in order to be at school by 7:30.
On Friday and Saturday nights he tries to stay out later but really struggles to stay awake. After the football games, he has tried to attend a few parties but can’t seem to stay awake. Mason often takes a nap or two on each weekend day.
Expert Insights
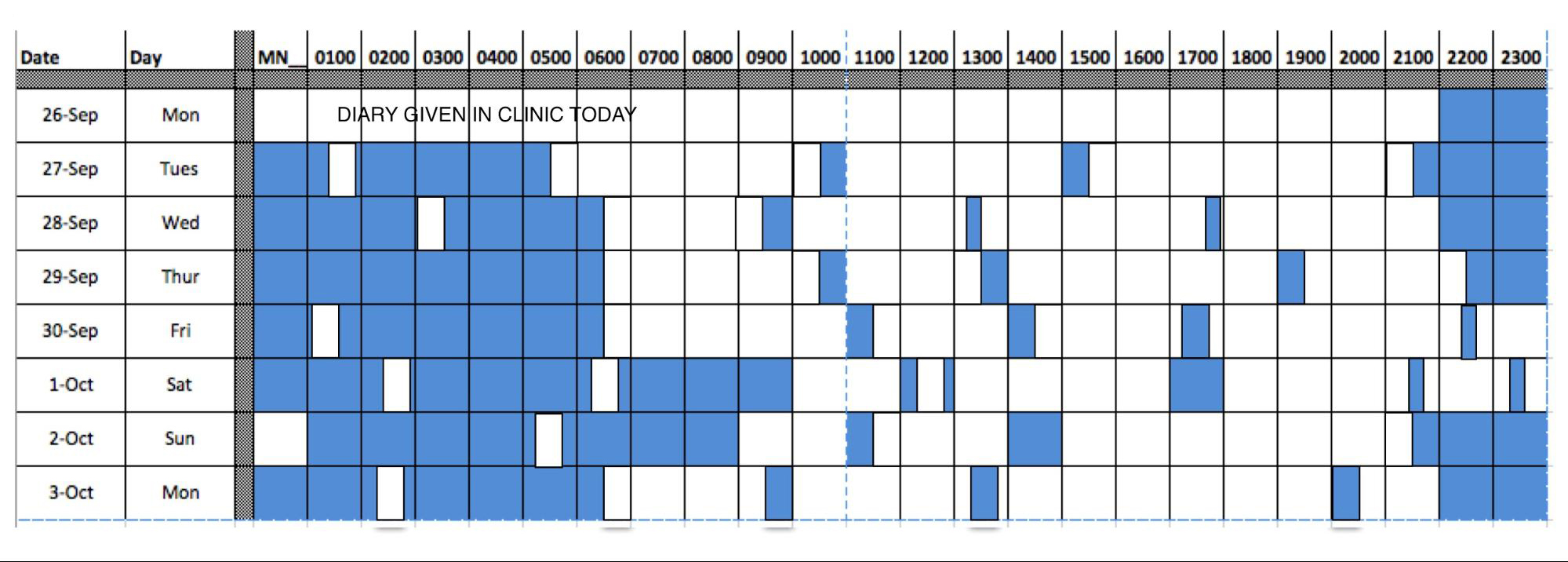
- Mason is obtaining 9 hours of sleep during the week and approximately the same amount during the weekends. This makes the diagnosis of insufficient sleep syndrome less likely. His story can be further confirmed with the use of actigraphy or a sleep diary.
- Mason’s sleepiness compromises his ability to socialize. Even with insufficient sleep syndrome, patients rarely give up social events or extracurriculars.
Mason’s mother notes that he occasionally snores at night. This usually occurs when he has an upper respiratory infection. He does not snore nightly.
Expert Insights
Given Mason’s weight (BMI of 28.9kg/m2 = 97th percentile) Mason is at risk for having sleep-disordered breathing or obstructive sleep apnea (OSA). While his mother’s recollection of his snoring only rarely makes it less likely, the history of daytime sleepiness and rare snoring needs to be further assessment with an overnight polysomnogram (sleep study).
- All patients evaluated for hypersomnia must undergo nocturnal polysomnogram prior to a mean sleep latency test to screen for other sleep disorders, such as periodic limb movement disorder or sleep apnea.
Mason's Evaluation & Diagnosis
What evaluation & diagnostic protocol should be used to diagnose Mason’s excessive daytime sleepiness?
Consider his triage vitals:
- Height 170.5 cm (67 in)
- Weight: 83.9 kg (185 lbs)
- BMI: 28.9 kg/m2 (97th percentile)
- BP 124/66 HR 74
- RR 16 Oxygen saturation of 99%
Check all that apply:
The evaluation protocol strategies we recommend for Mason's case are:
- Determine the child’s sleep history
- Perform physical examination
- Complete a Sleep Diary
- Refer to a sleep lab to obtain an overnight polysomnogram (Sleep Study) with a possible mean sleep latency study (MSLT)
- Refer to a Specialist
Mason needs to be evaluated with a comprehensive sleep history including assessment of his time asleep, frequency of naps, and use of medications. Additionally, history about cataplexy, hallucinations when falling asleep, or sleep paralysis should be obtained. A physical exam is also important to rule out other neurologic causes of sleepiness and weakness. A sleep diary, while not critical to the case, adds additional information that will allow a more rapid diagnosis of his disease. Finally, the sleep study and MSLT are of critical importance to evaluate Mason’s sleep at night. If the sleep study does not find the cause of his daytime sleepiness, then the MSLT will allow for the further evaluation of his sleepiness.
Determine Mason's sleep history
| Sleep History | Case Specific Information | Mason's Evaluation Results |
|---|---|---|
What the child does at night |
What does Mason do prior to going to bed? |
Mason comes home from football, takes a shower, eats dinner, and then does his homework. After homework he texts with his friends and girlfriend until he falls asleep. |
Review timing of events at night (bedtime/wake time) |
What time does Mason go to bed during the week? What time does he fall asleep? What time does he wake up in the morning? |
On Friday and Saturday nights he tries to stay out later, but really struggles to stay awake. After the football games, he has tried to attend a few parties but can’t seem to stay awake. |
Is this different on the weekend? |
Mason often takes a nap or two on each weekend day. |
|
Review timing of events at night (bedtime/waketime) |
Does Mason take naps during the day? If so for how long does he sleep? Does he feel refreshed after a short 15-20 minute nap? Does Mason snore? |
Mason takes a nap in the afternoon on the weekends and after school, if it is not during football season. He feels refreshed after even a short 15 minute nap. His mother has noticed that he snores occasionally. |
Review of medications: |
Is Mason taking medications like antidepressants, seizure medications, or antihistamines that might make him sleepier during the day? |
Mason is not taking any medications or illicit drugs. |
Does obstructive sleep apnea or narcolepsy run in the family. |
No. |
|
Does the patient have a history of feeling weak or have loss of muscle tone during episodes of laughing, crying, or excitement? |
His older brother and the older brother’s friends posted videos of Mason to social media this summer of him having “spells.” They told him jokes and when he laughed really hard, he fell down. |
|
Does the patient ever see things that are not present when falling asleep or when first awakening? |
Mason reports sometimes seeing his football coach standing over his bed as he falls asleep. |
|
Does the patient every wake up and feel like he is paralyzed, or is not able to move? |
No. Mason has never felt this way. |
|
Does the patient ever fall asleep during the day? |
Yes. Mason falls asleep at least twice per day. |
Perform physical exam
| Information to obtain includes: | Case Evaluation Results |
|---|---|
A comprehensive physical examination that targets organ systems of significance should be performed. In this case the HEENT, cardiac, respiratory and neurological systems should be assessed as each one of these could contribute to the child’s symptoms of daytime sleepiness. |
Mason is obese with a BMI at the 97th percentile. His neck is 17.5 inches in circumference. His throat examination reveals 1+ tonsils and Mallampati scale of 2. His neck is supple. Cardiac examination reveals normal pulses 2+ and no murmurs with a normal S1 and S2. Chest examination reveals bilaterally clear lung fields with no increased work of breathing. No wheezes. GI: Abdomen is soft, non-tender, non-distended with normal bowel sounds. Neuro examination: No focal deficits noted with 5/5 bilateral upper and lower extremity strength. |
Obtain an Epworth Sleepiness Score
| Information to obtain includes: | Case Evaluation Results | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
The Epworth Sleepiness Scale is a validated instrument to assess the level of sleepiness. The patient rates themselves from 0 (would never doze) to 3 (high chance of dozing) on their likelihood of falling asleep in eight different situations. A score greater than 10 suggests the presence of excessive sleepiness (Johns MW. Sleep. 1991, 14:540). The Epworth has been weakly correlated with MSLT scores. |
Mason completed the Epworth Sleepiness Scale.
|
Complete a Sleep Diary
| Information to obtain includes: | Case Evaluation Results |
|---|---|
|
A sleep diary allows the patient and family to document their sleep schedule. They are asked to mark the diary at time they fell asleep, and the time the awoke each day. The results allow for the assessment of sleep duration, time in bed and time asleep. The diary can be helpful in demonstrating the patient’s sleep schedule to the patient and family to encourage them to have earlier bedtimes or more consistent routines. |
Mason was given a sleep diary. He returned with it after one week. The diary suggests that Mason has a typical bedtime around 9:15 PM and he wakes at 6:30 AM during the week. He takes multiple naps throughout the day and stays up later on the weekends. 
|
Refer to a Sleep Lab
| Information to obtain includes: | Case Evaluation Results | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
A sleep study is indicated for evaluation of patients daytime sleepiness and to rule out OSA. A mean sleep latency test also should be performed. |
|
Refer to a Specialist
| Information to obtain includes: | Case Evaluation Results |
|---|---|
Consider visiting a sleep specialist. |
Referral to a sleep specialist is indicated for Mason due to the strong suspicion for Narcolepsy. |
Options that are Not Recommended
Patient with excessive daytime sleepiness should be evaluated in a timely fashion. Patient and family concerns should always be taken seriously.
Red Flags
- Patients and caregivers should have a detailed sleep history obtained whenever there is a complaint of excessive daytime sleepiness. This history may enable the diagnosis of insufficient sleep syndrome without any further costly testing or referral.
- A patient with excessive daytime sleepiness and history of cataplexy, sleep paralysis, or hallucinations should be referred for an evaluation with sleep study and MSLT to evaluate for narcolepsy.
- Patients with insufficient sleep syndrome, fragmented sleep due to sleep-disordered breathing, or periodic limb movements do not typically feel refreshed after a short 15-30 minute nap. Patients with narcolepsy often feel refreshed after a short nap.
- If a patient is experiencing daytime sleepiness and is noted to have abnormalities on a neurologic examination, such as cranial nerve deficits, consider other central neurologic diseases, such as malignancy.
When evaluating a child for possible hypersomnia, consider how other health care providers may also need to be involved.

- Cataplexy or the loss of muscle tone in response to emotional situations, especially laughter, is a near pathognomonic feature of narcolepsy, type 1.
- An Epworth Sleepiness Scale score greater than 10 is considered abnormal and should be further evaluated.
- The MSLT mean +/- SD in minutes is 11.6 +/- 5.2 minutes for adults and 16.2 +/- 1.5 minutes for teenagers. The MSL for patients with narcolepsy is 3.1 +/- 2.9 minutes. Unfortunately, MSLT cannot be applied in children who are less than 8 years old.
Evaluation & Diagnosis
What diagnosis is consistent with Mason's daytime sleepiness?
Check all that apply:
Mason’s signs and symptoms are consistent with the diagnosis of:
- Narcolepsy, type I
In this case, Mason's daytime sleepiness is not normal for his age, nor is it consistent with Insufficient sleep syndrome or Obstructive sleep apnea.
Mason is experiencing excessive daytime sleepiness as evidenced by his history, sleep diary, and Epworth Sleepiness Scale. He is also having episodes of cataplexy as seen by the videos that his brother obtained and the history of feeling weak on the football field. Mason is also experiencing hypnagogic hallucinations (hallucinations when falling asleep) of his football coach being in his bedroom. His MSLT is also diagnostic of narcolepsy as his MSLT is less than 8 minutes and he has 2 sleep onset REM periods visualized. Additionally, his REM latency of less than 15 minutes on the sleep study suggests the disease.
If the MSLT had been equivocal then further lab assessment may be warranted. HLA typing for DQB1*0602 could be obtained. DQB1*0602 is more prevalent in patients with narcolepsy with cataplexy, but it is also frequently found in the general population.
If the diagnosis were in doubt, then a cerebrospinal fluid (CSF) hypocretin level could be obtained. Hypocretin, also known as orexin, is a hypothalamic hormone that is decreased in patients with narcolepsy, type 1. It is a wake promoting hormone that also suppresses REM. Patients with narcolepsy, type 1, have CSF hypocretin levels less than 110 pg/ml or less than ⅓ of the normal value of the standardized assay.
Mason's Treatment & Referrals
Now it’s time to recommend treatment options for Mason.
Check all that apply:
Treatment Strategies for Narcolepsy
Patients with narcolepsy benefit from a combination of pharmacological and behavioral approaches.
The following treatment strategies are recommended for Mason:
- Refer to sleep Medical Provider
- Start a selective serotonin receptor inhibitor.
- Initiate stimulant therapy.
- Recommend frequent short naps.
Non-pharmacologic Treatments
Maintain adequate sleep at night. Teenagers should obtain at least 9 hours of sleep per night. Patients with narcolepsy should also plan to take a 15-20 minute nap in the afternoon. Weight management should be addressed to include eating a well balanced diet to help slow the rate and rise of BMI. Weight gain should be monitored closely and patients may need further nutrition intervention. Data suggests that regular exercise helps to prevent daytime sleepiness. Patients should be screen for coexistent depression. Additionally, patients who are in school should be advised to sit in the front row of class to increase awareness. Children and parents should be informed about safety concerns such as limiting activities that may provoke cataplexy and result injury (ie. monkey bars). Driving should be limited and well-supervised. Alcohol should be avoided.
Pharmacologic Treatment
Most patients with narcolepsy benefit from treatment with medications that promote wakefulness.
- Stimulants: Medications such as methyphenidate, dextroamphetamine are commonly used to treat patients with narcolepsy.
- Methylphenidate: Commonly used medication. It inhibits reuptake of dopamine and catecholamines and may enhance serotonin transmission as well. Common side effects include reduction in appetite, nausea, headache and insomnia. This is also a Schedule II controlled substance in the U.S.
- Amphetamine and dextroamphetamine: Sympathomimetic stimulants that cause the release of norepinephrine and dopamine and result in increased wakefulness. They may decrease cataplexy events as well. Side effects include reduced appetite, nausea, headache, insomnia, seizures, cardiovascular events.
- Modafinil and Armodafinil are used for mild to moderate daytime sleepiness. These medications have a less extensive side effect profile than the amphetamine stimulant categories of therapy. Modafinil and armodafinil have the common side effects of headache, anxiety, nausea, interference with oral contraceptives, and insomnia. Rare, but severe side effects include a severe rash.
Treatment for cataplexy
- Antidepressants are the cornerstone of therapy for cataplexy. Cataplexy is the result of REM sleep intruding into waking life. Both norepinephrine and serotonin suppress REM sleep and are useful in treating cataplexy.
- The use of SSRIs, which decrease REM sleep, is the primary treatments. Additionally, SSRIs in combination with SNRIs seem to have improved efficacy.
- Venlafaxine is a serotonin-norepinephrine reuptake inhibitor that is a first line therapy for cataplexy. Venlafaxine’s side effects include transient nausea, headache, insomnia, hypertension.
- Fluoxetine is also used to decrease symptoms of cataplexy and has the side effects of nausea, dry mouth, and insomnia.
- Clomipramine is a tricyclic antidepressant that effectively limits REM sleep and is a treatment of cataplexy. Side effect concerns include anticholinergic effects, dizziness, somnolence, weight gain, orthostatic hypotension, seizures, and cardiotoxicity.
Sodium Oxybate
- This is the sodium salt of gama-hydroxybutyrate. This is a highly sedating liquid that is given at bedtime and again 2.5 to 4 hours later. This medication produces deep stage N3 sleep. The mechanism is thought to be activation of GABA receptors. It can produce nausea, dizziness, urinary incontinence, sedation, and anxiety. Sodium oxybate has a high abuse potential and providers and patients must be registered before using this therapy.
Positive airway pressure is not needed in this case as he does not have sleep-disordered breathing or OSA.
When to consult a sleep specialist or refer to another discipline:
- The diagnosis of narcolepsy either with or without cataplexy likely should be confirmed by a board certified sleep physician. The sleep specialist can lead the diagnosis and develop a treatment plan for patients with narcolepsy.
Interdisciplinary Treatment Components

Mason's Results:
Good news! Mason was successfully diagnosed with narcolepsy, type 1, and the appropriate therapies were initiated.
Treatment strategies and results for Mason's narcolepsy:
- Mason was given a letter to allow him to take a short nap at school after lunch for 15 minutes.
This was made possible by having a “504 Plan” in place at school (see Resources & Clinical Tools for an example). This has markedly helped his grades improve as well as his daytime function. Mason is much more cognizant of continuing a consistent sleep pattern from the weekday and weekend. - Mason was started on modafinil 100 mg po every morning.
SInce starting modafinil, Mason has had a marked improvement in his ability to stay awake during the day. His Epworth scale has improved to 4 at his most recent clinic visit. - Mason started on venlafaxine at 37.5 mg every morning for his cataplexy.
Mason’s cataplexy has improved and he is not feeling weak while on the football fields. Sadly, for his brother, Mason no longer falls down when he begins to laugh. - Mason continues to work on diet and exercise.
He continues to play football, and the whole family has made a commitment to work on healthy eating habits.
Mason will need continued follow up with his sleep team to maintain his therapies, assess his risk of side effects, and to encourage him to continue to follow a rigorous treatment plan. Additionally, Mason has been instructed to consider careers that would be more stimulating, such as teaching, and to shy away from more sedentary careers that may further precipitate his sleepiness.
Mason’s sleep team referred him to his local Vocational Rehabilitation counselor. The counselor will assist Mason evaluate his strengths and preferences for college and career options. Mason really wants to go to college far away from home, but his parents want him to live at home so they can continue helping him manage his narcolepsy. He and his family will have to keep talking this over with the sleep team as he adjusts to his diagnosis and medication.
Mason really wants to get his learner’s permit to drive, but the sleep team decides to see how he does on medication for a few months before giving a medical clearance for “behind-the-wheel” training.